 There have been a lot of developments in the last few weeks around Medicaid expansion in Nebraska. The Nebraska Department of Health and Human Services has announced a series of choices they made that will delay Medicaid expansion’s rollout until 2020, implement a series of complex and costly work requirements, and reduce coverage options for current Medicaid enrollees.
There have been a lot of developments in the last few weeks around Medicaid expansion in Nebraska. The Nebraska Department of Health and Human Services has announced a series of choices they made that will delay Medicaid expansion’s rollout until 2020, implement a series of complex and costly work requirements, and reduce coverage options for current Medicaid enrollees.
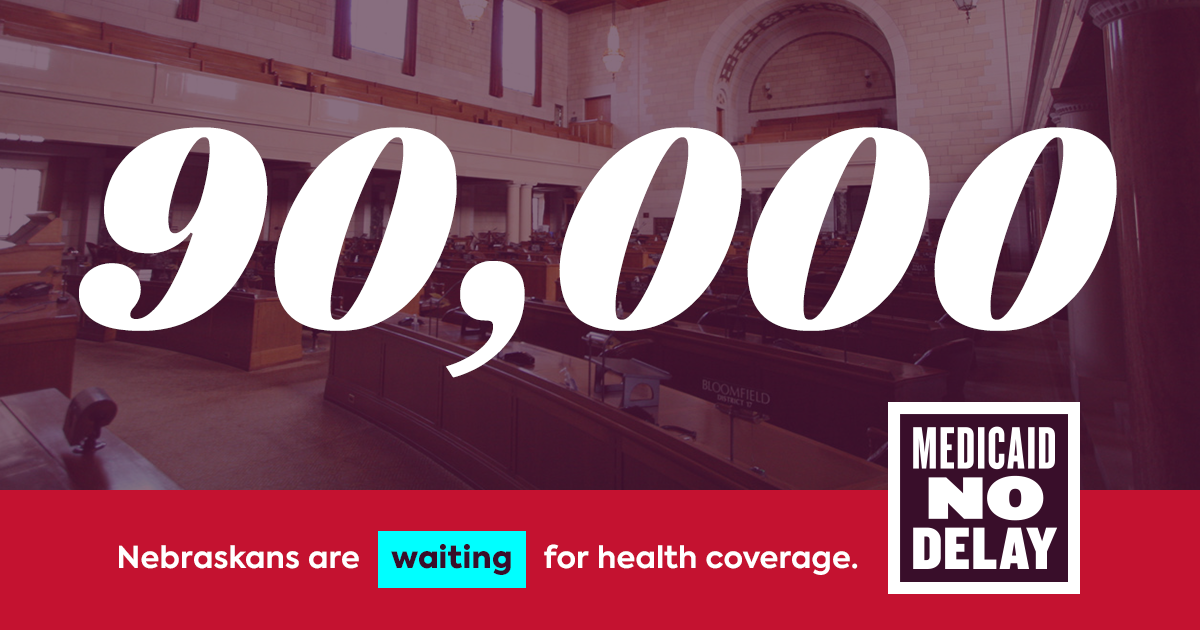
On April 1, the Nebraska Department of Health and Human Services (DHHS) filed the necessary state plan amendments (SPAs) to expand Medicaid in our state. These filings set the foundation for Medicaid expansion but also included a coverage start date of October 1, 2020. This coverage start date is around 23 months after voters passed Initiative 427. Nebraska voters passing Initiative 427 demonstrated an understanding of the health and financial challenges that result from not having insurance. However, under the DHHS plan for implementation, Nebraskans in the coverage gap continue to wait for coverage.
Along with the SPAs, DHHS also released a concept paper for a Section 1115 waiver project. A Section 1115 waiver is a demonstration project to deliver Medicaid in a way that is different from how Medicaid normally operates. Because it is a plan that deviates from traditional Medicaid law, it requires negotiation with and approval from the federal government. A Section 1115 waiver also requires public hearings and a notice and comment period and can take several months to be approved by the federal government.
Nebraska DHHS’s proposed Section 1115 waiver includes many elements. Specifically, the proposal would create the Heritage Health Adult Program, which would cover both adults eligible for Medicaid expansion and around 25,000 adults currently enrolled in Medicaid as parents or caretaker relatives. The Heritage Health Adult Plan would include a tiered benefits system with two levels of coverage called Basic and Prime.
- Basic Coverage would include the Medicaid benefits package minus dental, vision, and over the counter drugs.
- Prime Coverage would include dental, vision, and over the counter drugs.
To get Prime Coverage, Medicaid enrollees would have to engage in wellness requirements including choosing a primary care provider and completing an annual check up and, during the second year of the program, complete work requirements for 80 hours/month. The work requirements could be met through employment, participation in job search activities through the State of Nebraska, post-secondary education or apprenticeship, or volunteering through a public charity.
Adults currently eligible for Medicaid (those who aren’t becoming eligible through expansion) will be eligible for Prime Coverage during their first enrollment period (first six month of coverage). However, if Medicaid enrollees do not meet the requirements for Prime Coverage during their first enrollment period, they would receive Basic coverage for the next enrollment period. This means that the 25,000 adults currently enrolled in Medicaid could receive fewer benefits than they do now as a result of these program changes.
The proposed waiver would also modify a number of other areas of Nebraska’s Medicaid program:
- Redeterminations: Currently, Medicaid enrollees must re-verify their eligibility annually. The proposal would require eligibility redeterminations every six months.
- Early and Periodic Screening, Diagnostic, and Treatment (EPSDT): Medicaid provides a more robust benefits package for children through age 21. EPSDT is a comprehensive set of diagnostic, treatment, and preventive services currently provided to individuals up to age 21. As part of the waiver, DHHS is requesting to only provide that coverage up to age 19.
- Retroactivity: Currently, Medicaid eligibility is retroactive for up to three months prior to the date an individual enrolls in Medicaid if the individual would have been eligible for Medicaid during that period had they applied. DHHS is proposing to limit retroactive coverage to go back only to the first day of the application month for most groups enrolled in Medicaid, except pregnant women, children under 1 year old, and individuals in nursing facilities. Changes to retroactive coverage can have a significant negative financial impact on patients and providers.
This waiver proposal is complicated. It’s important to note that these proposed changes that reduce coverage, add needless complexity, and increase administrative costs were not contemplated or required by the ballot initiative passed by voters in November 2018. This waiver project is a choice; it is not something that we as a state must do to expand Medicaid. The SPAs filed on April 1 create the foundation for Medicaid expansion in Nebraska and are the only steps required by the initiative to expand Medicaid.
In coming months, your voice will be needed
to make sure Medicaid expansion is implemented as voters intended.
Call your state senator and urge them to tell DHHS to implement Medicaid expansion quickly and without work requirements and benefits changes voters did not authorize.
If you are personally affected by these proposed changes or waiting for Medicaid expansion and would like to take action, we would love to hear from you at coveragegap@neappleseed.org or 402-249-2492.


The poor are ALREADY WORKING!!! So, looks like everyone will get the premium plan. What amazes me is that our state officials still believe that the poor are unemployed lazy worthless losers. What is going to hit DHHS smack in the keester is that the majority of these 90K already have full time jobs, but because their pay is such a substandard, non living wage their income qualifies them for Medicaid.
The others are in need of Medicaid because they can’t find those jobs.
Why does this plan of Nebraska’s REEK of hate for the poor, prejudice and an utterly shaming definition of what they obviously believe is “the worthy poor.” I’m heartbroken that my state officials just proved they are full of hate and prejudice and false beliefs regarding the poor.
Not only that, their main complaint of enacting this before was the cost- the unnecessary additions to it actually make it MORE COSTLY. In all honesty I’m a little biased as I’m one of these people in a tough situation desperately needing health care, but I’m so sick of people treating the poor and unhealthy like they got themselves into the situation. Sure some did, but some of us were just born into Medicaid families and had lots of issues before being tossed out of Medicaid, but didn’t qualify for disability with the unreasonable expectation of full medical documentation that we can’t afford. I work a nearly full-time job but have to call in about once a week due to my issues, making it to where I don’t have enough hours for benefits through the company and I definitely could not afford marketplace health care considering half the time I only make 8-10k in a year.
I’ve already contacted who I can about this but my illnesses make it very difficult to contact people through phone call, so I hope those who can are making those calls.
Nebraska Appleseed should sue Nebraska DHHS and Ricketts because the “work requirement” waiver, which is intended to deny Medicaid coverage to as many people as possible, has been tried in Arkansas and Kentucky and both of these states LOST in court. Apparently Nebraska DHHS needs to be taken to court in the same way in order to quit trying to sabotage healthcare for people that need it. In Arkansas many WORKING people were automatically dropped because the required verification was onerous. That was it’s intent, and those state’s governments and governors were called on the carpet. Some people on Medicaid can’t work- and the 2 tier coverage “Basic” and “Prime” are shameful. People currently on Medicaid will suffer, as well as the intended expansion population. Why hasn’t a lawsuit been filed already?